The health and recovery of people with serious diseases can be negatively affected by a condition called critical illness myopathy (CIM). This sort of muscular weakness typically occurs alongside additional consequences in the setting of serious disease. Here, we’ll examine the ins and outs of critical illness myopathy, including its origins, manifestations, diagnostic tools, and therapeutic options. Let’s read below “Critical Illness Myopathy and Its Effects”:-
Understanding Critical Illness Myopathy
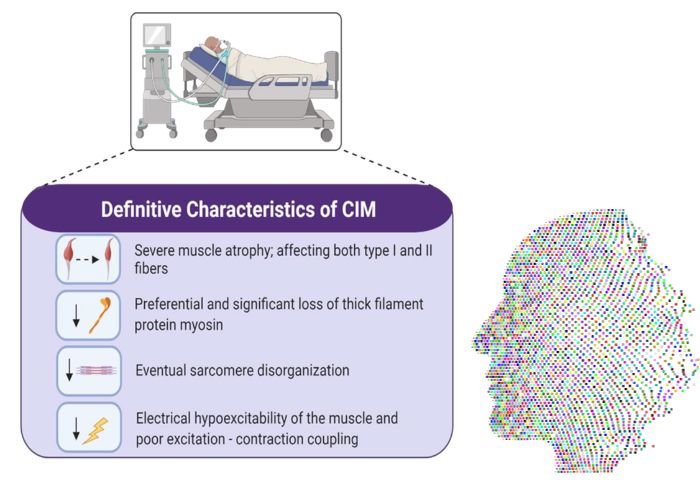
Serious disease myopathy is a neuromuscular condition marked by significant muscle weakness that occurs in critically unwell people. The skeletal muscles are predominantly affected, and these are the muscles used for all voluntary actions, including walking and grasping. Patients in intensive care units (ICUs) with life-threatening conditions such severe infections, trauma, or respiratory failure frequently have this syndrome.
Critical Illness Myopathy and Its Effects
Although its precise origins remain unknown, various risk factors have been recognized for critical disease myopathy. The systemic inflammatory response that occurs with critical diseases is a major precipitating factor. When muscles become inflamed, a chain reaction can begin, one of which is the activation of pathways that tear down muscle tissue.
Another risk factor for the development of critical illness myopathy is the prolonged immobilization and bed rest that is typically required in intensive care units. Muscle atrophy and weakening can result from inactivity. A higher chance of acquiring this illness has also been linked to the use of certain drugs, including corticosteroids and neuromuscular blocking agents.
Effects on the Body
Myopathy caused by a severe disease might have serious consequences for the body. Muscle weakness is the most recognizable sign and can vary in severity. Patients may have trouble breathing, moving, or standing on their own. Extreme instances may render patients incapable of even the most fundamental of everyday tasks.
The mental toll of critical disease myopathy can be just as severe as the physical ones.The time it takes to get better might be quite a bit longer than expected.
Diagnostic Approaches
- Diagnostic Challenges:
- Diagnosing critical illness myopathy is challenging due to symptom similarities with other neuromuscular diseases.
- A thorough evaluation is necessary to eliminate other potential causes of muscle weakness.
- Comprehensive Evaluation Process:
- Full assessment includes:
- Detailed analysis of medical history.
- Extensive physical examination.
- Laboratory tests aimed at excluding alternative reasons for muscle weakness.
- Full assessment includes:
- Electromyography (EMG) and Nerve Conduction Studies:
- Evaluation of muscle and nerve electrical activity is commonly done through EMG and nerve conduction studies.
- These assessments aim to identify specific patterns indicative of muscular dysfunction associated with critical illness myopathy.
- Muscle Biopsies for Confirmation:
- To confirm a diagnosis, muscle biopsies are often performed.
- This involves the removal of tissue, which is then examined under a microscope.
- The microscopic examination helps in verifying the presence of critical illness myopathy.
Treatment Strategies
It takes a multidisciplinary team of doctors and nurses working together to effectively treat critical illness myopathy.
1. Physical Therapy: rehabilitation is essential for people with critical disease myopathy to make a full recovery. Strengthening muscles, increasing range of motion, and enhancing general function are all goals of physical therapy. Key components of therapy include range-of-motion exercises and progressive mobilization.
2. Respiratory Support: Mechanical ventilation may be required to aid breathing in patients with severely compromised respiratory muscles. This treatment is essential for avoiding hypoxia and respiratory collapse.
3. Nutritional Support: Thirdly, nutritional support is essential for maintaining healthy muscles and speeding their recovery. Patients in critical care often suffer from malnutrition, and treating these deficits can improve muscular function.
4. Monitoring Medications: Medical professionals need to keep a close eye on patients taking any drugs, but especially those that might cause or exacerbate muscular weakness. This involves reassessing the usage of neuromuscular blocking drugs and corticosteroids.
5. Addressing Underlying Conditions: Fifth, it’s important to treat the underlying medical condition that brought on severe sickness myopathy. Components of the treatment plan include the aggressive management of infections, the treatment of injuries, and the improvement of general medical care.
Prognosis and Challenges
Individuals with critical illness myopathy have a range of prognoses, based on factors such as the severity of their disease, the nature of their underlying illness, and the efficacy of their therapy. Even after receiving treatment, some individuals may continue to suffer from muscular weakness and other functional difficulties.
The absence of a definitive diagnosis and therapy for critical illness myopathy is one of the major obstacles to effective patient care. The illness is generally part of a complicated clinical picture involving many organ systems, needing a thorough and tailored approach to management.
Research and Future Directions
The only way we will ever learn enough about critical disease myopathy to create effective new treatments is if we keep digging.
Improving outcomes for people with critical disease myopathy requires clinical trials investigating the effectiveness of innovative therapies, such as particular medications or rehabilitation methods. Improved diagnosis accuracy and treatment recommendations may result from ongoing research into the identification of biomarkers for early detection and monitoring of the illness.
Conclusion
One of the more difficult aspects of providing intensive care is dealing with myopathy brought on by severe illness.
As our understanding of the underlying processes continues to advance, so too will our capacity to create tailored therapies that improve outcomes for patients affected by critical illness myopathy. Until then, it is essential to provide each person with this severe illness with individualized, comprehensive supportive care and rehabilitation. I hope you like reading “Critical Illness Myopathy and Its Effects.”